
Carbonic Anhydrase Inhibitor Mechanism Of Action Pdf
Papich DVM, MS, DACVCP, in, 2016 Pharmacology and mechanism of actionMethazolamide is a carbonic anhydrase inhibitor. Methazolamide, like other carbonic anhydrase inhibitors, produces diuresis through inhibition of the uptake of bicarbonate in proximal renal tubules via enzyme inhibition. This action results in loss of bicarbonate in the urine and diuresis. The action of carbonic anhydrase inhibitors results in urine loss of bicarbonate, alkaline urine, and water loss. Methazolamide, like other carbonic anhydrase inhibitors, also decreases formation of cerebrospinal fluid (CSF) by the choroid plexus and decreases the ocular fluid formation by decreasing bicarbonate secretion by the ocular ciliary body. This effect on aqueous humor formation decreases ocular pressure.
Carbonic anhydrase inhibitors may produce acid-base and electrolyte alterations. These alterations were not reported in the clinical trials with brinzolamide. However, in patients treated with oral carbonic anhydrase inhibitors, rare instances of acid-base alterations have occurred with high-dose salicylate therapy.
Marsden, in, 2018 AcetazolamideAcetazolamide is a carbonic anhydrase inhibitor that causes CO 2 to accumulate within the brain, blocking anion transport and increasing γ-aminobutyric acid (GABA) levels, leading to a modulation of firing rate ( Wyllie et al., 2010). It is also used as an antiepileptic. Case reports suggest that acetazolamide decreases the number of attacks in episodic ataxia 2 in 66% of cases ( Jen et al., 2004; Ilg et al., 2014).
An open-label study of acetazolamide in 6 people with SCA6 for 88 weeks demonstrated improvements in postural sway and ratings of ataxia. Improvements plateaued after 48 weeks ( Yabe et al., 2001). Yan Luo, in, 2013 Treatment Pharmacological treatmentThe successful treatment of schisis cavities with carbonic anhydrase inhibitor has been previously reported. 111 Genead et al. 112 treated 29 eyes of 15 XLRS patients with topical dorzolamide for 4–41 months and noted some positive effects on visual acuity, cystoid macular lesions, and central foveal thickness.
Further studies are required to elucidate the true frequency and completeness of the response to dorzolamide, as well as to evaluate for possible recurrence of foveal cystic change. 113 More specific pharmacotherapies may become possible as the pathogenetic mechanisms of XLRS are better understood. LaserLaser photocoagulation is often considered as an adjuvant or preventive treatment for XLRS.
114,115 However, scatter laser photocoagulation performed in order to flatten peripheral schisis cavities and reduce the likelihood of retinal detachment resulted in retinal detachment in many cases. 116 So the administration time and effectiveness of laser treatment for XLRS should be carefully considered. SurgerySurgical intervention may be required for XLRS patients with severe complications, such as retinal detachment and vitreous hemorrhage.
Currently, the main surgeries include scleral buckle, 115 vitrectomy, and perfluorocarbon liquid, perfluorodecalin or sulfur hexafluoride gas tamponade. Vitreous surgery includes core vitrectomy, surgical induction of posterior vitreous detachment, removal of the internal limiting membrane, and gas tamponade.
117In addition, Wu et al. 118 used autologous plasmin enzyme-assisted vitreoretinal surgery to treat XLRS patients and achieved retinal reattachment in 91% (20/21) of eyes and postoperative visual improvement in 53% (8/15). Gene therapyGene therapy also holds great promise for the treatment of inherited retinal degenerations.
119 Gene therapy might be an effective treatment for XLRS patients. 120 The RS1 gene delivered intraocularly in RS1-knockout mice was found to restore b-wave amplitude of the treated mice. 121,122 XLRS patients may benefit from the replacement of RS1 gene, even at advanced stages, and gene replacement may be a promising treatment for XLRS patients in the near future. 123 Retina and/or progenitor cell transplantationRetinal transplantation or replacement also holds promise as a potential future therapy for XLRS disease in conjunction with the development of new surgical techniques and instrumentation.
However, due to the limited source of human tissue and ethical considerations, it is important to find an alternative cell source for retinal replacement therapy. Transplantation of stem cells and/or progenitor cells, including retinal progenitor cells, bone marrow-derived cells, and induced pluripotent cells, may eventually provide an alternative approach to restore vision. 124 Compared to human embryonic stem cells, the use of human bone marrow-derived cells and induced pluripotent cells does not have significant ethical issues and may eliminate the risk of immunorejection.
▪ Clinical Pharmacology:M echanism of A ction: A carbonic anhydrase inhibitor that reduces formation of hydrogen and bicarbonate ions from carbon dioxide and water by inhibiting, in proximal renal tubule, the enzyme carbonic anhydrase, thereby promoting renal excretion of sodium, potassium, bicarbonate, and water. Ocular: Reduces rate of aqueous humor formation, lowers intraocular pressure. T herapeutic E ffect: Produces anticonvulsant activity.P harmacokinetics: Rapidly absorbed. Protein binding: 95%. Widely distributed throughout body tissues including erythrocytes, kidneys, and blood-brain barrier.
Not metabolized. Excreted unchanged in urine. Removed by hemodialysis. H alf-life: 2.4-5.8 hr. ▪ Indications and Dosages:G laucoma: PO 250 mg 1-4 times/day.
Extended-Release: 500 mg 1-2 times/day usually given in morning and evening.S econdary glaucoma, preop treatment of acute congestive glaucoma: PO/IV 250 mg q4h, 250 mg q12h; or 500 mg, then 125-250 mg q4h.E dema: IV 25-375 mg once daily.E pilepsy: Oral 375-1000 mg/day in 1-4 divided doses.A cute mountain sickness: PO 500-1000 mg/day in divided doses. If possible, begin 24-48 hr before ascent; continue at least 48 hr at high altitude. Initially, 250 mg 2 times/day; use lowest effective dose.D osage in renal impairment. Karin Jurkat-Rott. Frank Lehmann-Horn, in, 2015 Periodic Paralyses: Therapeutic InterventionsTherapeutic studies of the periodic paralyses have so far only been performed with dichlorphenamide, 64 a carbonic anhydrase inhibitor no longer available.
With normokalemic periodic paralysis patients, avoidance of dyskalemia and medication with carbonic anhydrase inhibitors is a suitable prophylaxis against paralytic episodes. Patients with hypokalemic periodic paralysis should avoid food rich in carbohydrates and strong bodily work.
They should eat food rich in potassium (see above) and low in sodium. To avoid paralytic episodes, medication with carbonic anhydrase inhibitors like acetazolamide and/or the aldosterone antagonist eplerenone is recommended ( Figure 38.13). Potassium saving diuretics like triamterene or amiloride would also be suitable, but in certain countries they are only available in combination with potassium-excreting diuretics; this, of course, counteracts their effect. The dose of the drugs should be slowly increased (e.g. In adults, eplerenone should start with 25 mg/d and be increased to 50 mg/d in the second week; the dose will need adjustment in children based on weight).
Safety has been established in children younger than 18 years of age. 65 A combination of carbonic anhydrase inhibitors, potassium-sparing diuretics, and potassium, each at low dosage, may reduce the side effects of the drugs.
With this combination, the possibility of hyperkalemia with muscular weakness and cardiac arrhythmias exists, which persists until the hyperkalemia is reversed. The danger of this possibility happening is, however, much lower than feared by many physicians, because most of the patients present even in the interval with serum potassium values at the lower norm, and the potential of eplerenone to cause hyperkalemia is extremely low in contrast to the formerly used spironolactone. In fact, it turns out to be rather difficult to raise their serum potassium level to a persisting 4.8 to 5.2 mM, values that would suffice to let them experience less muscle weakness, less muscle pain, and a reduced number of paralytic episodes.In some patients, carbonic anhydrase inhibitors have an opposite effect: for reasons unknown they lead to an increase in the number and severity of paralytic attacks. 66 Aldosterone antagonists and potassium-sparing diuretics are helpful in these cases. 6 In an acute episode, at least, potassium should be administered. The aforementioned drugs are also effective in antagonizing the lasting muscle weakness, provided muscle tissue is still preserved.
6 Since it has been shown that potassium may repolarize the depolarized muscle fibers of patients with hypokalemic periodic paralysis, potassium should not only be given during a paralytic episode, but also as a prophylactic measure. This may sound paradoxical, but often it works! Best suited are slow-retard potassium tablets.
6 A thyrotoxic hypokalemic periodic paralysis is best cured by treating the hyperthyroidism. In an acute case, potassium and carbonic anhydrase inhibitors may be used. 13 Some experts also advocate beta-blockers.In Andersen-Tawil syndrome, carbonic anhydrase inhibitors can be used as prophylactic means against paralytic attacks. Extrasystoles should not be treated at any cost; often the arrhythmias disappear with tachycardia, as with moderate bodily stress or fever. A treatment with blockers of the sodium or calcium channels or with beta-blockers is common but often not effective. Earlier investigators reported imipramine as useful.
Amiodarone should be given only in severe cases because of its substantial side effects. For the long-QT syndrome, this drug is even contraindicated. 67 In cases of arrhythmogenic syncope, a pacemaker or a combined pacemaker/defibrillator may be indicated.
All drugs that prolong the QT time are strongly contraindicated. Utter, Dennis E. Brooks, in, 2011 Topical or Oral Carbonic Anhydrase InhibitorAqueous humor production can also be reduced if 99% of the carbonic anhydrase enzyme in the ciliary body is inhibited. The carbonic anhydrase inhibitor, dorzolamide (2%), alone or in combination with timolol maleate was effective in lowering IOP by 10% (2 mm Hg) when administered topically twice a day in normal horses. 22 Once-a-day use increased IOP in normal horses in another study.
21 Brinzolamide, a carbonic anhydrase inhibitor associated with fewer side effects in people, most likely due to a physiologic pH (relative to dorzolamide, which is acidic), has been shown to decrease IOP following once- and twice-daily topical administration of a 1% solution in normal horses. 23 Neither topical carbonic anhydrase inhibitor has been used in a controlled study with glaucomatous horses.Acetazolamide, dichlorphenamide, and methazolamide are systemically administered carbonic anhydrase inhibitors that have been used to reduce IOP in other species, but the pharmacokinetics have been studied only for acetazolamide in horses. In horses, when acetazolamide is given orally, it is absorbed rapidly and has somewhat lower bioavailability, but it is eliminated more slowly than when it is administered intravenously. 24 Acetazolamide has been shown to reduce clinical signs of hyperkalemia in horses with hyperkalemic periodic paralysis when given at 4.4 mg/kg twice daily, but no studies have evaluated the effect of acetazolamide on IOP in either normal or glaucomatous horses. Administration of systemic carbonic anhydrase inhibitors should be accompanied by electrolyte supplementation because of presumed potassium loss. Polak, in, 2005 DorzolamideAdverse effects associated with systemic carbonic anhydrase inhibitors have adversely affected adherence to treatment in patients with glaucoma, obviating their long-term use. The tolerability and efficacy of dorzolamide, a topical carbonic anhydrase inhibitor, has been studied in a selected group of 39 patients with glaucoma and ocular hypertension, who were intolerant of systemic carbonic anhydrase inhibitors in a 3-month prospective study (21 c).
The patients were evaluated on the day of switching from systemic carbonic anhydrase inhibitor to dorzolamide and at five more visits. Within 4 weeks after switching the mean health assessment scores improved significantly in seven of the eight categories of the SF-36 questionnaires, used to evaluate changes in well-being and quality of life. There were no significant differences between the mean intraocular pressure on day 0 and subsequent measurements. In patients with glaucoma who are intolerant of systemic carbonic anhydrase inhibitors, topical treatment with dorzolamide offers similar efficacy and better tolerability.
Robin G Stanley, in, 2008 Carbonic anhydrase inhibitorsCarbonic anhydrase inhibitors (CAIs) are extremely useful in reducing intraocular pressure by about 15 mmHg. They reduce aqueous production by inhibition of carbonic anhydrase. Dozolamide (Trusopt®, MSD) is the topical carbonic anhydrase inhibitor used most frequently in managing glaucoma in dogs and cats. Other topical CAIs are brinzolamide (Azopt®, Alcon) and dorzolamide/timolol (Cosopt®, MSD).In veterinary ophthalmology this class of drug is most useful in treating glaucoma that is secondary to uveitis or hyphema and following luxated lens removal. They do not seem to be effective in treating acute, primary glaucoma.
Robert L Stamper MD. Michael V Drake MD, in, 2009Carbonic anhydrase inhibitors (CAIs) continue to be the only systemic agents used for the long-term treatment of glaucoma, if only occasionally.
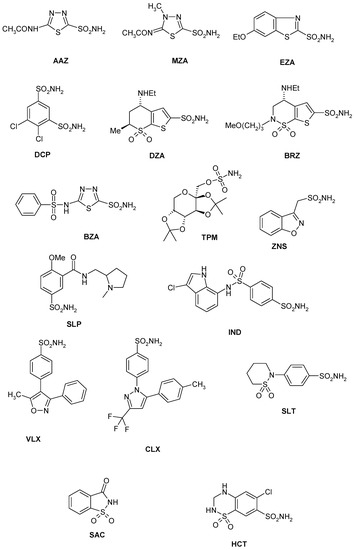
A topical version introduced more than 40 years after the introduction of the systemic agent moved the oral agents quite far down on the list of practical options for the chronic treatment of glaucoma. These drugs are all derivatives of sulfonamides and were introduced into clinical practice as diuretics. Even with chronic use, their diuretic action is only effective for 1–2 weeks.
CAIs reduce intraocular pressure (IOP) by decreasing aqueous humor formation. As such they are useful in essentially all forms of glaucoma, even when the anterior chamber angle is sealed or the outflow facility is very low. SummaryCarbonic anhydrase inhibitors are IOP-lowering sulfonamide derivatives which inhibit the activity of CA in the ciliary processes of the eye, thus reducing aqueous humor formation and consequently decreasing IOP. Systemic CAIs provide an approximately 40% IOP reduction, and their effect develops rapidly. Therefore, systemic CAIs (most frequently acetazolamide) are useful to break acute angle-closure glaucoma and to reduce high IOP prior to filtering surgery. However, when used chronically, systemic CAIs have many systemic side effects. Indeed, some side effects of acetazolamide can even be lethal. Andaaz movie online.
In contrast, the topical CAIs dorzolamide and brinzolamide are safe systemically, and their side effects are mostly local. In monotherapy, the IOP decrease achieved with either of these topical CAIs varies between 15% and 20%, a figure which is considerably less than the reduction produced by acetazolamide. In clinical practice, topical CAIs are mainly used as a part of a combined IOP-lowering medication.
Their additional IOP-lowering efficacy is especially favorable when they are added to nonselective β-receptor blockers or prostaglandin analogues. The IOP reduction provided by the topical CAIs is stable over long usage, with no long-term drift phenomenon. In order to increase the ocular penetration, dorzolamide is formulated with an acidic pH, which may explain the more frequent and severe local side effects as compared to brinzolamide. All CAIs influence ocular perfusion, but the clinical significance of the CAI-induced increase of ocular blood flow remains to be specified. At present, the information on the altered ocular perfusion due to CAI administration cannot be interpreted as evidence of IOP-independent retinal ganglion cell protection in glaucoma. Jeffries, Dennis W. Wolff, in, 2017 Therapeutic usesCarbonic anhydrase inhibitors can be used to treat the edema of congestive heart failure but are no longer widely used for this purpose.
When used to treat edema, best results are obtained when the drug is skipped every other day or every 2 days, giving the kidneys an opportunity to recover lost HCO 3 –. Carbonic anhydrase inhibitors also suppress aqueous humor formation in the eyes and can be used to reduce intraocular pressure in open-angle glaucoma and before surgery in cases of angle-closure glaucoma. Treatment of glaucoma is the therapeutic indication for most carbonic anhydrase inhibitors that are now on the market. For reasons that are not well established, but perhaps because of the tendency toward acidosis with these drugs, carbonic anhydrase inhibitors are also useful for treating epilepsy (especially absence seizures in children).
A final use for these drugs is the treatment of altitude sickness when taken before the ascent and, if necessary, to suppress symptoms for a few days afterward. Koeppen MD, PhD, Bruce A. Stanton PhD, in, 2013 Carbonic Anhydrase InhibitorsCarbonic anhydrase inhibitors (e.g., acetazolamide) reduce Na + reabsorption by their effect on carbonic anhydrase. This enzyme is abundant in the proximal tubule and therefore represents the major site of action of these diuretics. Carbonic anhydrase also is present in other cells along the nephron (e.g., thick ascending limb of Henle’s loop and intercalated cells of the collecting duct), and administration of carbonic anhydrase inhibitors affects the activity of the enzyme at these sites as well. However, the effects of these diuretics are almost entirely attributed to their inhibition of the enzyme in the proximal tubule. This phenomenon reflects the fact that approximately one third of proximal tubule Na + reabsorption occurs in exchange for H + (through the Na +-H + antiporter) and thus depends on the activity of carbonic anhydrase (see Chapter 8).Even though one third of proximal tubule Na + reabsorption is coupled to the secretion of H +, inhibition of this process by the carbonic anhydrase inhibitors does not result in a large natriuresis for several reasons.
First, even with complete inhibition of carbonic anhydrase, some Na + reabsorption (linked to bicarbonate reabsorption) still occurs. Second, downstream nephron segments increase their reabsorption of Na + (e.g., the thick ascending limb, distal tubule, and collecting duct), and third, increased delivery of Na + to the macula densa leads to a reduction in the GFR by the tubuloglomerular feedback mechanism. Finally, with long-term administration, a metabolic acidosis develops, which further decreases the effect of carbonic anhydrase inhibitors by reducing the filtration of HCO 3 − (i.e., the percentage of Na + reabsorbed with HCO 3 − in the proximal tubule is reduced). Typically, administration of carbonic anhydrase inhibitors results in Na + excretion rates that are 5% to 10% of the filtered Na +. Robin G Stanley, in, 2008 Carbonic anhydrase inhibitorsCarbonic anhydrase inhibitors (CAIs) are extremely useful in reducing intraocular pressure by about 15 mmHg. They reduce aqueous production by inhibition of carbonic anhydrase.
Dozolamide (Trusopt®, MSD) is the topical carbonic anhydrase inhibitor used most frequently in managing glaucoma in dogs and cats. Other topical CAIs are brinzolamide (Azopt®, Alcon) and dorzolamide/timolol (Cosopt®, MSD).In veterinary ophthalmology this class of drug is most useful in treating glaucoma that is secondary to uveitis or hyphema and following luxated lens removal. They do not seem to be effective in treating acute, primary glaucoma. Carbonic anhydrase inhibitors can rarely cause Stevens–Johnson syndrome (9 A).A 62-year-old man with cerebrovascular disease underwent regional cerebrovascular reactivity to intravenous acetazolamide 1000 mg using single-photon emission computed tomography with 123I N-isopropyl-para-iodoamfetamine 0.45 mg. Three days later he developed erythematous eruptions of varying sizes on his back, which then spread over his entire body.
The presumptive diagnosis was Stevens–Johnson syndrome and he was given a glucocorticoid. The skin and mucous lesions became bullous or erosive, ruptured spontaneously, and dried with crusting. He gradually improved over 21 days. Lymphocyte transformation tests were positive with acetazolamide.All previous cases have occurred in patients taking oral acetazolamide for glaucoma and have been limited to Japanese or Indian patients or patients of Japanese descent, as was the case here.
Kwiatkowski MD, MS. Cooper MD, MPH, in, 2019 Other Diuretics.Carbonic anhydrase inhibitors (acetazolamide) are weak diuretics, with the main site of action in the proximal tubular lumen and cell. Blockade of carbonic anhydrase leads to decreased bicarbonate and sodium reabsorption via the Na +/HCO 3 − cotransporter, resulting in reduced water reabsorption.
They are most often used for the treatment of a significant metabolic alkalosis. Acetazolamide may promote nephrocalcinosis and nephrolithiasis when combined with loop diuretics. Osmotic diuretics (mannitol) act mainly in the proximal tubule. Mannitol undergoes glomerular filtration and is not reabsorbed along the tubular system.
Osmotic diuretics increase osmolality of the tubular fluid and subsequently water and sodium excretion. Mannitol results in a shift of extracellular fluid into the intravascular space in infants with low cardiac output and poor renal perfusion after cardiac surgery.
It therefore has the potential to exacerbate CHF and pulmonary edema in patients with myocardial dysfunction.A common complication of CHF is acute and chronic renal disease with hypervolemic hyponatremia. This can be attributed to venous congestion, decreased renal perfusion, and extended use of diuretics. Although diuretics are necessary, the associated electrolyte abnormalities may exacerbate hyponatremia by limiting the kidney's ability to excrete free water. Tolvaptan is an oral selective vasopressin V 2-receptor antagonist that induces hypotonic diuresis without affecting electrolytes. 144 The efficacy and safety of tolvaptan is established in adult patients. 144-147 A multicenter clinical trial of tolvaptan in children with euvolemic or hypervolemic hyponatremia is currently under way ( ClinicalTrials.gov, NCT02012959).
In, 2011 Carbonic Anhydrase Inhibitors Site of ActionCarbonic anhydrase inhibitors (CAIs) act primarily in the proximal tubule; an additional, albeit modest, effect along the distal nephron is also observed. Mechanism of ActionCAIs work by inhibition of luminal and cellular carbonic anhydrase, resulting in an alkaline diuresis with impaired reabsorption of Na +, Cl −, and HCO 3 − and decreased excretion of titratable acid and NH 4 +. There is substantial kaliuresis, although hypokalemia is uncommon.
Diuretic efficacy is limited by distal Na + and HCO 3 − reabsorption and development of metabolic acidosis, which limits the filtered load to HCO 3 −, thereby curtailing natriuresis. Most diuretics have some carbonic anhydrase activity. PharmacokineticsAcetazolamide (Diamox) is readily absorbed. It is eliminated by tubular secretion (which is diminished by hypoalbuminemia), and has a half-life (t 1/2) of 13 hours. Methazolamide (Neptazane) has less plasma protein binding, a longer t 1/2, and greater lipid solubility, all of which favor penetration into aqueous humor and cerebrospinal fluid (CSF). It has fewer renal effects and therefore is preferred for treatment of glaucoma.
Clinical IndicationsThe use of CAIs is limited by their transient action, development of metabolic acidosis, and a spectrum of adverse effects. They can be used with NaHCO 3 infusion to cause an alkaline diuresis that increases the excretion of weakly acidic drugs (e.g., salicylates and phenobarbital) or acidic metabolites (urate).
Chloride-responsive metabolic alkalosis is best treated by administering Cl − with K + or Na +. However, if this produces unacceptable extracellular volume (ECV) expansion, acetazolamide (250–500 mg/day) and KCl can be used to increase HCO 3 − excretion. These agents are useful in glaucoma by diminishing the transport of HCO 3 − and Na + by the ciliary process, thereby reducing the intraocular pressure. CAIs also limit formation of CSF and endolymph. Acetazolamide is used in a dose of 250 mg twice daily as prophylaxis against mountain sickness, probably through stimulating respiration and diminishing cerebral blood flow. In established mountain sickness, it improves oxygenation and pulmonary gas exchange. It can stimulate ventilation in patients with central sleep apnea.
CAIs are effective in prophylaxis of hypokalemic periodic paralysis due to diminished influx of K + into cells. Paradoxically, they are also useful in the treatment of hyperkalemic periodic paralysis. Adverse EffectsLethargy, abnormal taste, paresthesia, gastrointestinal distress, malaise, and decreased libido are among the adverse effects seen with treatment. Administration of NaHCO 3 may ameliorate symptoms, but increases the risk of nephrocalcinosis and nephrolithiasis, which is tenfold higher in patients receiving acetazolamide. Symptomatic metabolic acidosis develops in 50%; the elderly, diabetics, and patients with chronic kidney disease (CKD) may develop serious metabolic acidosis. An alkaline urine favors partitioning of renal ammonia into blood, rather than its elimination in urine, and may precipitate encephalopathy in patients with liver failure.
Avinash Kulkarni. ET Cunningham Jr, in, 2015 Carbonic Anhydrase Inhibitors and Hyperosmotic Agents.Topical carbonic anhydrase inhibitors are widely used in uveitic glaucoma and often as part of a dorzolamide-timolol fixed combination. In some uveitics, largely those with a chronic history and probable severe ciliary body damage, drugs such as dorzolamide and brinzolamide may profoundly reduce IOP. Although this is not necessarily a contraindication, lower doses than normal may be required.Acetazolamide is frequently used to manage acute rises in IOP in uveitis patients if topical therapy proves inadequate. It is especially helpful in combination with topical therapy for treatment of refractory cases pending definitive surgery. Hyperosmotic drugs such as mannitol and glycerol are rarely indicated.
Price, in, 2018 Carbonic Anhydrase InhibitorThe carbonic anhydrase inhibitors (acetazolamide) are relatively weak diuretics and are used mainly for the treatment of glaucoma. This class of diuretics acts by decreasing sodium and bicarbonate reabsorption in the proximal tubule. When carbonic anhydrase in the tubular cell is blocked, water reabsorption is deceased and a concomitant loss of bicarbonate in the urine results in a metabolic acidosis within 2–4 days of therapy 4. This effect may be desirable and useful in heart failure patients who develop a hypochloremic metabolic alkalosis while being treated with loop diuretics. In a study of 74 adult patients with severe congestive heart failure and hypochloremic metabolic alkalosis while treated with furosemide, a combination of acetazolamide and spironolactone was administered for hypochloremic metabolic alkalosis 29. Most of the patients experienced significant weight loss, even when furosemide dosing was held briefly, as well as correction of the metabolic abnormality.